Psoriasis is a chronic autoimmune skin condition that is much more common than many people realize. While it might not always make headlines in the world of skincare, it affects about 125 million people worldwide.
If you’ve ever wondered whether those mysterious red patches or stubborn scales on your skin could be a sign of something more, you’re not alone. In this blog, we’ll shed light on psoriasis, its common symptoms, potential causes, and the importance of seeking professional advice if you suspect you might have it. Psoriasis doesn’t discriminate, and understanding its presence in your life can make a world of difference in your journey toward clearer, healthier skin.
What is Psoriasis?
Psoriasis is a chronic skin condition characterized by the body’s immune system mistakenly attacking healthy skin cells. Imagine your immune system as the body’s defense mechanism, like an army protecting your skin. In psoriasis, this defense system gets confused and starts attacking the skin itself. As a result, your skin cells reproduce much faster than usual, piling up on the surface. This rapid cell turnover leads to the formation of red, raised patches covered with silvery-white scales. It’s as if your skin is trying to heal a wound that isn’t there.

Common Symptoms of Psoriasis
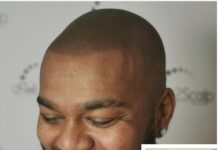
The most common symptom of psoriasis is the appearance of these distinct red patches, which can be slightly elevated. These patches often develop a silvery, scaly layer, which distinguishes psoriasis from other skin conditions. While they can appear anywhere on the body, psoriasis commonly affects areas like the elbows, knees, scalp, lower back, and sometimes even the nails. These patches can be itchy, painful, or both, and their severity can vary from person to person. Understanding these symptoms is crucial for early diagnosis and effective management.
It’s very common for people with psoriasis to have concerns about how it appears on their skin, given its visible nature. But, it’s crucial to know that psoriasis is nothing to be ashamed of. Like we said above, it’s a common skin condition affecting millions of individuals worldwide, and it doesn’t discriminate. It’s not your fault that you have it or due to anything you have (or haven’t done) as part of your skincare routine. Understanding and accepting this can help remove the stigma associated with.
And if you believe you have it, you shouldn’t be worried about being judged when you go visit a dermatologist. Seeking proper medical care and support is vital, as managing psoriasis effectively is entirely achievable. Your dermatologist will be understanding and ready to help you with psoriasis treatment.
Possible Causes and Triggers
Understanding why psoriasis happens for each individual can be a bit like solving a puzzle. While the exact cause remains a mystery, experts believe it’s linked to both genetics and the immune system. Think of it as a family trait and your body’s defense system going slightly overboard.
Psoriasis can be a bit sensitive too. It doesn’t always act up, but certain triggers can make it flare. Stress, infections like strep throat, and specific medications can all play a role. Knowing what might set off your psoriasis can be a game-changer in managing it effectively, so definitely mention it to your dermatologist when you have your consultation.

What To Expect During Your Clinic Visit
First, the dermatologist will conduct a thorough physical examination. This includes closely inspecting your skin, scalp, and nails for the telltale signs of psoriasis, such as red, raised, scaly patches. These patches often appear on elbows, knees, scalp, and lower back but can manifest anywhere on the body. The dermatologist may also inquire about your family history, as psoriasis can be hereditary.
Next, the dermatologist will ask about your symptoms and medical history. This conversation is crucial as psoriasis can sometimes be associated with other health conditions like psoriatic arthritis, type 2 diabetes, and cardiovascular issues. The doctor might ask about the duration of your symptoms, any known triggers or exacerbating factors, and how the condition impacts your daily life.
In some cases, to confirm the diagnosis, the dermatologist might perform a biopsy. This involves taking a small sample of skin tissue to examine under a microscope. The biopsy helps differentiate psoriasis from other similar skin conditions, such as eczema or fungal infections.
Common Psoriasis Treatments
Topical treatments are often the first line of defense for psoriasis, especially in milder cases. These can include corticosteroids, which reduce inflammation and redness, vitamin D analogues that slow skin cell growth, and moisturizers for dry skin. There are also topical retinoids, calcineurin inhibitors, and coal tar preparations, each with specific benefits and use cases.
For more severe or extensive cases of psoriasis, or when topical treatments are insufficient, light therapy (phototherapy) might be recommended. This involves exposing the skin to ultraviolet light under medical supervision. The most common form of light therapy uses narrow-band UVB light, which can slow skin cell turnover and reduce scaling and inflammation. Another type, PUVA therapy, combines UVA light with a medicine called psoralen to achieve similar effects.
Systemic medications are typically reserved for the most severe cases or when psoriasis is resistant to other treatments. These can be oral medications like methotrexate or cyclosporine, which suppress the immune system, or newer biologic drugs that target specific parts of the immune system to reduce inflammation and skin cell turnover. These biologics are often administered via injection and have transformed the treatment landscape for severe psoriasis, offering hope for better symptom management.
In addition to these medical treatments, lifestyle adjustments and self-care techniques play a crucial role in managing psoriasis. Dermatologists often advise patients to maintain a healthy weight, avoid tobacco and excessive alcohol, and manage stress, as these factors can exacerbate psoriasis symptoms. Regular moisturizing can alleviate dry skin, and avoiding harsh soaps or skin products can prevent irritation. Sun exposure in moderation can also be beneficial, but it’s important to avoid sunburn, which can worsen psoriasis.
In some cases, your dermatologist might also recommend dietary changes. While there is no specific diet for psoriasis, some patients find that certain foods can trigger flare-ups. Keeping a food diary to identify and then avoid these triggers can be helpful.
Overall, the treatment and management of psoriasis are highly individualized, and what works for one person may not work for another. Regular consultations and open communication with a dermatologist are essential to finding the most effective treatment plan

Taking the First Step
Taking the first steps toward psoriasis treatment can be difficult, though the support you’ll receive from your doctor and the comfort you’ll feel as your symptoms subside will be well worth it. Living with psoriasis might have its challenges, but it’s not something to be afraid of or ashamed about. With the right combination of therapies tailored to your needs, you’ll have fewer flare-ups, worry less, and enjoy a much greater sense of well-being.